Ah – there’s nothing like a good night’s rest to make you ready to take on the day. But if you often wake up feeling exhausted – even after clocking in a full night’s sleep – you might be one of the millions of Americans who suffer from sleep apnea.
Sleep apnea can disrupt your breathing and rob you of restful sleep. While many brush it off as a nuisance, untreated sleep apnea can have serious consequences for your health, including irregular heartbeat, high blood pressure, heart disease and stroke.
So how can you tell if you are at risk? Kristin Mock, MD, specializes in sleep medicine at OSF HealthCare. She offers insight to help you find out if sleep apnea is affecting your sleep, and what to do about it.
What is sleep apnea?
Ready to sleep better?
Sleep apnea is a very common disorder affecting people of all ages. It causes brief interruptions of breathing during sleep called “apneic events.”
There are three types of sleep apnea:
- Obstructive sleep apnea: This is the most common type and happens when an obstruction blocks airflow.
- Central sleep apnea: This happens when the brain fails to send the right signals to the muscles to start breathing.
- Complex sleep apnea: This is a combination of both obstructive and central apneas.
Sleep Apnea Risk Factors
Sleep apnea often runs in families. You are more likely to develop it if you:
- Snore loudly
- Are overweight
- Have high blood pressure
- Have a physical abnormality in the nose, throat or other part of the airway
If you have sleep apnea, using alcohol or sleeping pills can increase the frequency and duration of breathing pauses.
Common Symptoms of Sleep Apnea
Sleep apnea symptoms can be hard to pinpoint at first, but there are key patterns to watch for. These include: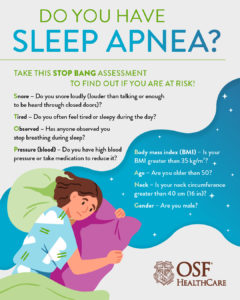
- Loud, chronic snoring: While not everyone who snores has sleep apnea, intense snoring often indicates an underlying issue.
- Pauses in breathing during sleep: No matter which type of sleep apnea you have, your breathing pauses during sleep, as many as several hundred times a night in severe cases.
- Waking up gasping for air: This may feel like a choking sensation. When breathing restarts, you may snort or gasp.
- Excessive daytime fatigue or morning headaches: Pauses in breathing break up deep, restorative sleep.
“It can also be common for those with sleep apnea to go to the bathroom a lot during the night,” says Dr. Mock. “They may be woken up, not realizing their breathing has been interrupted, and think they need to go to the bathroom or get a drink.”
Sleep Apnea in Children
Up to 6% of children in the U.S. have obstructive sleep apnea. Children with ADHD, autism and Down syndrome have a much higher rate of sleep disorders, including sleep apnea.
Sleep apnea in children can be harder to detect because the typical signs adults experience are often absent.
“Often children don’t snore loudly, and don’t complain of being tired or sleepy to their parents,” says Dr. Mock. “Instead, they might have mood dysfunction, poor concentration and be restless sleepers.”
Some of these symptoms may indicate other conditions, so it’s important to talk with your child’s provider.
Sleep Apnea Tests: What You Need to Know
If you or your partner suspect you might have sleep apnea, your primary care provider can refer you to a sleep specialist. There are several types of tests to evaluate your sleep, including:
- Sleep Study (Polysomnography): This is done in a sleep lab and measures brain waves, eye movement, heart rate and breathing patterns during sleep.
- Home Sleep Apnea Test (HSAT): A portable device that is worn during sleep at home and returned to your doctor to process the results. Children are typically not candidates for this test.
“Home sleep apnea tests are convenient, but a normal test doesn’t necessarily mean you don’t have sleep apnea,” says Dr. Mock. “Sometimes there can be false negatives, so you should follow your home test with an in-lab sleep study, which is more thorough.”
Your doctor will help you determine which sleep apnea test is right for you, and work with your other providers to share results and decide what to do next.
Can wearables help detect sleep apnea?
Technology continues to evolve, and many people are turning to wearable devices to help them monitor their health, including sleep patterns. However, none of these devices are designed to specifically diagnose sleep apnea.
But wearables and apps can be useful tools for getting information about your sleep. There are many devices with a variety of different features, including:
- Smart watches: Devices like the Apple Watch or FitBit can help monitor your sleep patterns and detect potential warning signs of sleep apnea. Worn on the wrist, these devices provide information on heart rate and oxygen levels. Some FitBit models can track snoring using the device’s microphone to detect noise, including snoring from you or someone next to you.
- Smart rings: Devices like the Oura ring or Ultrahuman ring, are a convenient way to monitor and potentially detect signs of sleep apnea. Worn on the finger, these devices track blood oxygen levels and sleep quality.
“If you are concerned about any sleep data your wearable device is showing, it’s a great place to start a conversation with your doctor,” says Dr. Mock. “These devices are not as accurate as an in-lab sleep study. Your provider can help you take steps to find out if you have sleep apnea, how severe it is and what to do about it.”
When should you see a doctor about sleep apnea?
If you suspect you have sleep apnea, talking with your primary care provider early on can help prevent complications later. Your provider can review your symptoms and refer you to a sleep specialist for further evaluation. They can set you up with testing and offer treatment recommendations based on your age and how severe your condition is.
It’s probably time to schedule an appointment with your doctor if:
- You consistently experience symptoms like daytime sleepiness, loud snoring or waking up gasping for air.
- A wearable device consistently shows patterns like low oxygen levels or irregular sleep cycles.
- If either of the above are true, and you have high blood pressure, heart problems or other related conditions.
Last Updated: April 23, 2025
